
Write something
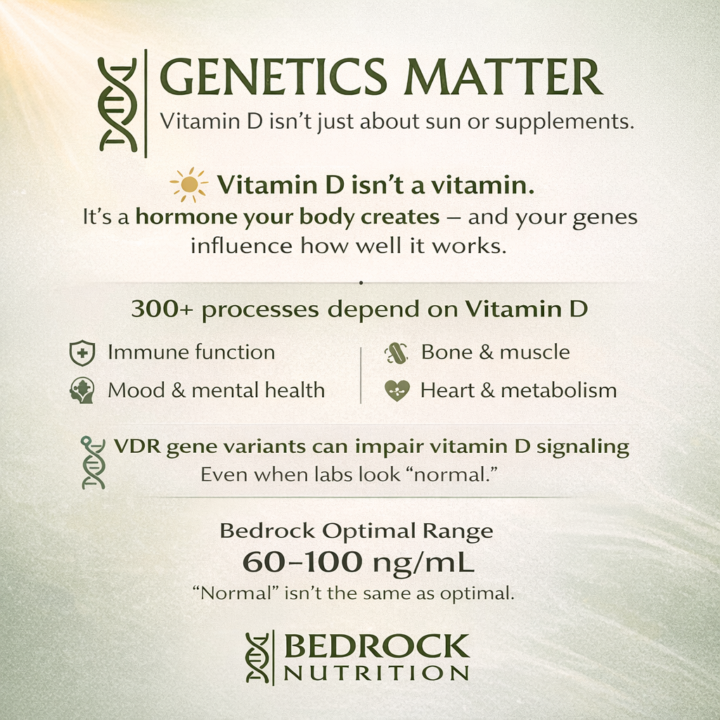
Vitamin D: More than a vitamin.
☀️ Vitamin D isn’t actually a vitamin. It’s a hormone your body creates, and it plays a role in far more than bone health. Vitamin D receptors are found throughout the body, and research shows vitamin D is involved in 300+ biological processes, including: • Immune resilience • Bone density & muscle function • Cardiovascular health • Mood regulation & mental health • Cognitive performance & brain health • Thyroid and metabolic signaling Yet here’s where most conversations stop short 👇 Having vitamin D present doesn’t always mean your body can use it effectively. 🧬 Genetics matter. Variations (SNPs) in the Vitamin D Receptor (VDR) genes can impair how well your cells respond to vitamin D — even if blood levels look “normal.” This means someone can: • Get sun exposure • Take supplements • Show a “normal” lab value …and still experience symptoms tied to functional vitamin D insufficiency. This is why we often pair vitamin D testing with genetic insight and symptom patterns — numbers alone don’t tell the whole story. 🔍 That’s why at Bedrock Nutrition, we don’t aim for minimum adequacy. We aim for optimized terrain. 📊 Our clinical target: Vitamin D (25-OH D3): 60–100 ng/mL Compare that to the conventional “normal” cutoff of ~30 ng/mL — a level that may still be associated with: • Low mood & depressive symptoms • Increased anxiety • Poor immune signaling • Thyroid dysfunction • Higher inflammatory burden This aligns with what leaders in brain health continue to emphasize. Dr. Daniel Amen recently highlighted that vitamin D deficiency is linked to hundreds of conditions, including depression, cognitive decline, autoimmune disease, and dementia — and that 3 out of 4 Americans now fall below optimal levels. 📌 Testing matters. We don’t guess. We measure — and we interpret in context. 👉 Take our functional health assessment: 🔗 https://adobe.ly/41cHOYw When levels are low or utilization is impaired, D3 paired with K2 becomes foundational for absorption, transport, and safety.
2
0
Neuroterrain is Live in the Classroom
I’m excited to officially open access to my Mental Health Terrain Course: Neuroterrain, inside Bedrock Nation, here on Skool. So many people are trying to “think” their way out of anxiety, depression, brain fog, irritability, burnout, and overwhelm—while the terrain underneath their brain chemistry is screaming for support. This course is a root-cause, practical, and hope-filled framework for strengthening mental wellness by addressing the foundations that influence mood and cognition, including: • Blood sugar + metabolic stability • Gut–brain + inflammation • Nutrient depletion + mitochondrial support • Sleep + circadian rhythm • Nervous system regulation + daily rhythm “anchors” • Strategic lab testing (when needed) If you’ve been looking for a step-by-step, non-fluffy approach that connects the dots between physiology, lifestyle, and resilience—this is for you (and for the families you serve). Join the classroom here: https://www.skool.com/bedrock-nation-8489/classroom/ab34cae5 #MentalHealth #FunctionalNutrition #RootCause #NervousSystem #Wellness BedrockNation AnxietySupport HolisticHealth
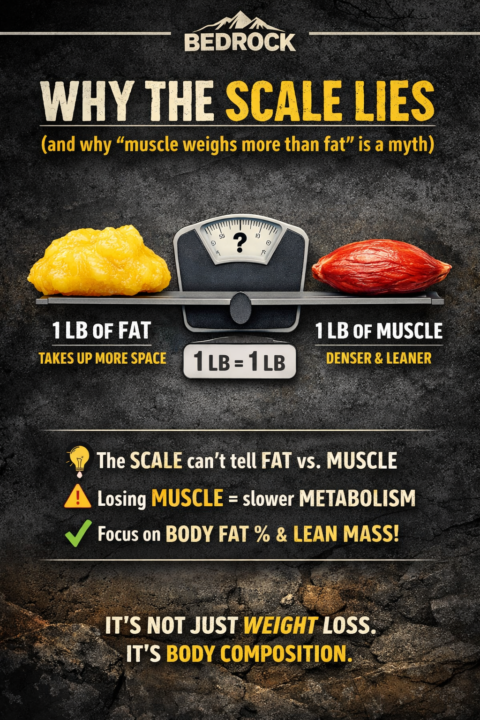
Why the Scale Lies (and the “Muscle Weighs More Than Fat” Myth Needs to Die)
If you’ve ever stepped on the scale after a week of “doing everything right” and thought, What is happening? — you’re not crazy. The scale is one tool… but it’s a limited tool. And first, we need to bust the myth that keeps people confused: Myth: “Muscle weighs more than fat.” Truth: 1 pound of muscle weighs the same as 1 pound of fat. A pound is a pound. The real difference is density. Muscle is denser than fat, which means pound-for-pound it takes up less space. That’s why two people can weigh the same and look completely different — and why you can “not lose weight” but still get noticeably leaner. What the Scale Actually Measures (and What It Doesn’t) Your scale measures total body mass. It does not tell you how much of that mass is: - fat - muscle - water - glycogen (stored carbs) - inflammation - food volume in your digestive tract So the scale can go up because: - you slept poorly - you’re under stress (hello cortisol + water retention) - you ate more sodium - you trained hard (muscle inflammation + fluid shifts) - hormones are shifting - you’re constipated or simply holding more food volume None of those automatically mean “you gained fat.” Why “Weight Loss” Can Make You Worse Off Most people think progress = scale down. So they: - cut calories harder - do more cardio - skip resistance training - under-eat protein The scale may drop quickly at first — but here’s the problem: If you lose weight fast, a meaningful chunk often comes from water + muscle, not fat. And losing muscle is a big deal because muscle is not just “for looks.” Muscle is metabolic armor. It helps with: - resting metabolic rate (burning more energy at baseline) - glucose disposal and insulin sensitivity - resilience as you age - strength, stability, joint support - recovery and stress tolerance So if the scale says you’re lighter, but you’re losing muscle, you may end up: - softer-looking at a lower weight - more fatigued - weaker in workouts - stalled with fat loss later - regaining weight more easily
5
0
Seed Oils - The Silent Saboteur
For decades we have been told these “vegetable” oils were safe, even “healthy.” But research shows that they are anything but! The Omega 6 fatty acids in seed oils are drivers of inflammation, insulin resistance and even cancer.
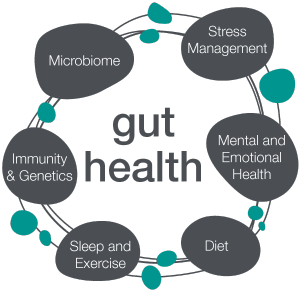
The Gut Health Crisis: What I’m Seeing Every Day (and What’s Really Going On)
If it feels like everyone is dealing with gut issues right now… you’re not imagining it. Across our Bedrock clients, the patterns are loud and consistent: - bloating that shows up out of nowhere - reflux that “randomly” flares - constipation (or the opposite) that becomes normal - food reactions that change week to week - fatigue, anxiety, skin issues, headaches, joint pain… with “normal” tests And that’s the most frustrating part: people are suffering, but standard workups often come back as “fine.” Here’s the truth from the trenches: gut dysfunction is common long before gut disease is diagnosable. The body can be struggling for months or years while labs stay within “normal” ranges. Why gut issues are exploding right now In most cases, it’s not one cause. It’s a pile-up. These are the top drivers I see repeatedly: 1) Ultra-processed food exposure Even people who “eat pretty healthy” are often getting hit with hidden emulsifiers, additives, refined oils, artificial sweeteners, and low-fiber convenience foods. That combination can: - reduce microbial diversity - increase gut irritation and cravings - destabilize blood sugar - keep inflammation simmering 2) Chronic stress and a dysregulated nervous system Your gut is not just a digestive tube. It’s a nervous system organ. When stress is chronic: - motility slows (constipation, bloating, SIBO-type patterns) - stomach acid and enzyme output can drop - the gut lining becomes more reactive - symptoms become “random” because your nervous system is the amplifier 3) Medications and modern exposures This is not judgment—this is reality. Common meds can change the terrain: - acid blockers - NSAIDs - repeated antibiotics - hormonal birth control - even certain sleep/anxiety meds Add in environmental exposures and it’s a lot for the gut barrier and microbiome to carry. 4) Sleep disruption and circadian chaos Late nights, artificial light, inconsistent routines, “revenge bedtime,” and caffeine loops don’t just affect energy.
1-19 of 19
powered by
skool.com/bedrock-nation-8489
Free wellness community for faith based living, functional health and real connection - off social media, rooted in purpose - learn, grow and heal.
Suggested communities
Powered by
