
Write something
Prevalence of Back Pain in UK Adults Aged 40–70 and Evidence-Based Therapy Outcomes
Prevalence - Low back pain is highly prevalent in UK adults aged 40–70, with ~25–30% reporting back pain within any given month. - Prevalence peaks in the early 50s, but remains consistently high through age 70. - Chronicity increases with age, leading to higher rates of persistent or recurrent symptoms in this demographic. Therapy Outcomes Exercise & Physiotherapy - Structured exercise programmes provide small to moderate improvements in pain and functional ability. - Best outcomes occur with supervised or group-based programmes and good adherence. - Exercise is consistently more effective than passive modalities. Psychological Interventions - CBT and ACT show strongest benefit when combined with physical rehabilitation. - Improvements are seen mainly in function, coping, and reduction in disability, rather than pain intensity alone. - Particularly valuable for chronic, non-specific low back pain. Manual Therapy - Provides short-term symptom relief for some patients. - Evidence supports its use as an adjunct, not a stand-alone treatment. - Most effective when it facilitates active rehabilitation. Interventional & Surgical Options - Injections: May benefit radicular or facet-related pain short term, but limited long-term impact. - Surgery: Most beneficial when a clear structural cause exists (e.g., radiculopathy, stenosis). Clinical Perspective - Adults aged 40–70 represent a high-burden group for persistent back pain. - Evidence supports a multidisciplinary, biopsychosocial approach combining education, exercise, behavioural strategies, and expectation management. - No single modality is curative; best outcomes occur when interventions are integrated and sustained. References 1. MacFarlane GJ, Beasley M, Jones EA, et al. The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain. 2012;153(1):27-32. DOI:10.1016/j.pain.2011.08.005 PubMed+1 2. National Institute for Health and Care Excellence (NICE). Low back pain and sciatica in over 16s: assessment and management. NICE guideline NG59. Published 30 Nov 2016, updated Dec 2020. Nice+2NCBI+2 3. Singh V, Parslow D, Smith R, et al. A systematic review and meta-analysis on the efficacy of physiotherapy interventions for low back pain. PMCID: PMC7934127. PMC 4. Tran TH, Schmitt Y, Deldon K, et al. Effects of cognitive behavioral therapy combined with physical therapy in patients with chronic low back pain. PMC article. PMC 5. Leung T-W, Chung R, Ma Y, et al. The effect of cognitive behavioural therapy on pain and disability in chronic non-specific low back pain: a systematic review. PLOS One. PLOS 6. NIHR Evidence. Cognitive behavioural therapy may help people with persistent low back pain. NIHR alert. NIHR Evidence 7. O’Keeffe M, Hayes S, O’Sullivan P, et al. Individualised cognitive functional therapy compared with a combined exercise and manual therapy intervention for chronic non-specific low back pain: a randomized controlled trial.BMJ Open. 2015;5(6):e007156. BMJ Open 8. Miki T, Kamper SJ, Roussel NA, et al. The effect of cognitive functional therapy for chronic low back pain: a systematic review and meta-analysis. BioPsychoSocial Medicine. 2022. BioMed Central 9. Rushton A, Heneghan NR, Heymans MW, et al. Clinical course of pain and disability following primary lumbar discectomy: systematic review and meta-analysis. European Spine Journal. 2020;29:1660–1670. Springer Link 10. Liu C, Tabaković I, Szetajnković M. Surgical versus non-surgical treatment for sciatica: systematic review. BMJ. 2023. BMJ 11. NHS / Local policy: Cheshire & Merseyside NHS. Spinal decompression for low back pain & sciatica policy. (Cites NICE NG59 for surgical selection.)
2
0
The Soleus Muscle: A Foundational Contributor to Locomotion and Running Efficiency
Among the triceps surae group, the soleus remains one of the most underappreciated muscles in clinical and performance discussions. While the gastrocnemius often receives primary focus for its visible contribution to plantarflexion and sprinting, the soleus — with its endurance-oriented fiber composition and unique mechanical role — is arguably the first major muscle group to engage in the kinetic chain during gait initiation and running. Anatomical and Functional Overview The soleus originates from the posterior aspect of the tibia and fibula and inserts into the calcaneus via the Achilles tendon. Unlike the gastrocnemius, it does not cross the knee joint, allowing for consistent activation regardless of knee angle. This monoarticular design enables the soleus to provide postural stability and generate sustained plantarflexion torque, particularly during stance and propulsion phases (Michaud, n.d.). The muscle’s composition is predominantly Type I slow-twitch fibers, making it highly fatigue-resistant and capable of sustaining prolonged contraction without rapid decline in force output (Böhm et al., 2021). This structural adaptation is critical for its continuous role in stabilizing the tibia over the talus and maintaining center-of-mass control throughout gait. Early Engagement and Mechanical Role in Gait During the stance phase of both walking and running, the soleus is among the first lower-limb muscle groups to engage following heel contact. It eccentrically controls tibial advancement over the foot, then transitions concentrically to provide propulsive force. Research using ultrasound and EMG data confirms that the soleus fascicles remain active throughout stance, operating near optimal shortening velocities for mechanical efficiency (Böhm et al., 2021; Lai et al., 2015). In running, this function becomes magnified. Sasaki and Neptune (2006) demonstrated that the soleus contributes substantially to both vertical support and forward propulsion, generating forces up to eight times body weight at push-off. These mechanical contributions occur with minimal metabolic cost due to its fiber type composition and tendon elasticity, highlighting its role in energy conservation during repetitive loading cycles.
1
0
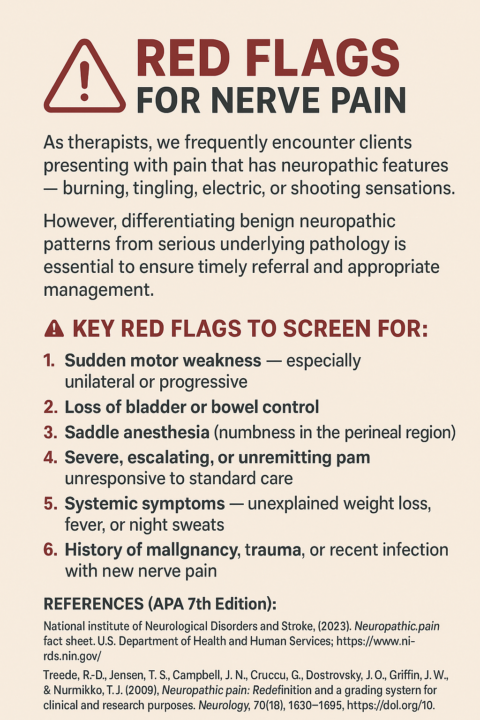
🧠 Recognising Red Flags for Nerve Pain in Clinical Practice 🚨
When these signs are present, immediate medical assessment is warranted to rule out conditions such as cauda equina syndrome, spinal cord compression, or systemic infection. As movement and rehabilitation professionals, our role isn’t only to alleviate pain but also to recognize when neurological compromise requires escalation. Early identification can significantly reduce morbidity and improve outcomes for our clients. 📚 References (APA 7th Edition): - National Institute of Neurological Disorders and Stroke. (2023). Neuropathic pain fact sheet. U.S. Department of Health and Human Services. https://www.ninds.nih.gov/ - Treede, R.-D., Jensen, T. S., Campbell, J. N., Cruccu, G., Dostrovsky, J. O., Griffin, J. W., & Nurmikko, T. J. (2008). Neuropathic pain: Redefinition and a grading system for clinical and research purposes. Neurology, 70(18), 1630–1635. https://doi.org/10.1212/01.wnl.0000282763.29778.59 - National Institute for Health and Care Excellence. (2020). Neuropathic pain in adults: Pharmacological management in non-specialist settings (CG173). https://www.nice.org.uk/guidance/cg173
2
0

Research into to post hamstring injury strength
Eccentric training is commonly used in rehabilitation and cohort/observational studies report favorable outcomes, yet randomized evidence directly showing superior percentage strength gains versus concentric‑only training is scarce. The randomized trial that compared a program including progressive running plus eccentric strengthening with an agility/trunk program found similar recovery and MRI outcomes at return to sport papers used [see references to expand]: - Eccentric cohort outcomes A lengthened‑state eccentric protocol (50 athletes) reported a reinjury rate of 8% (4/50) over follow‑up and measured isometric strength across multiple knee angles before return to sport - Individualized eccentric rehab In a group of 26 athletes with recurrent strains, individualized eccentric‑emphasis rehabilitation normalized isokinetic parameters in 17 of 18 subjects treated and produced zero clinically diagnosed reinjuries during 12‑month follow‑up - Residual deficits at RTS Several studies show residual concentric and eccentric deficits at the time of clinical return to sport (e.g., mean injured‑limb peak torque deficit 9.6% at RTS in one cohort), which often resolve over months - Systematic synthesis A meta‑analysis of 28 studies concluded that eccentric and concentric strength deficits can persist after hamstring strain and recommended monitoring dynamic (eccentric/concentric) strength at and after return to sport Muscle architecture and function: Muscle architecture and dynamic performance after hamstring strain have been measured in several studies, but numeric reports of fascicle length and pennation angle changes after eccentric versus concentric training are sparse. Imaging and performance studies show consistent qualitative patterns but limited precise comparative percentages. - Fascicle length Decreased biceps femoris long‑head fascicle lengths after injury and persistent shorter fascicles have been reported across studies and reviews, and eccentrically biased strengthening is recommended to address fascicle length deficits - Muscle volume and edema MRI findings in one cohort showed 20.4% of muscle cross‑sectional area with edema at RTS and a 4–5%reduction in muscle volume over 6 months - Pennation angle Specific reported numeric changes in pennation angle after eccentric versus concentric rehabilitation are not provided in the cited clinical trials and reviews; therefore quantitative comparison is insufficient evidence. - Functional performance Persistent deficits in eccentric knee‑flexor strength, reduced horizontal ground reaction forces in sprinting, and impaired repeated sprint ability have been observed after hamstring strain and are targeted by eccentrically biased and sport‑specific running programs
Poll
3 members have voted
1
0
1-5 of 5
powered by
skool.com/the-rehabilitation-academy-6086
Pain Excellence Programme. A place to build knowledge and apply in the real world. Therapy progression REAL cases with REAL results.
Suggested communities
Powered by
