
Write something
The Real Product of FirstCall DPC Isn’t Medicine
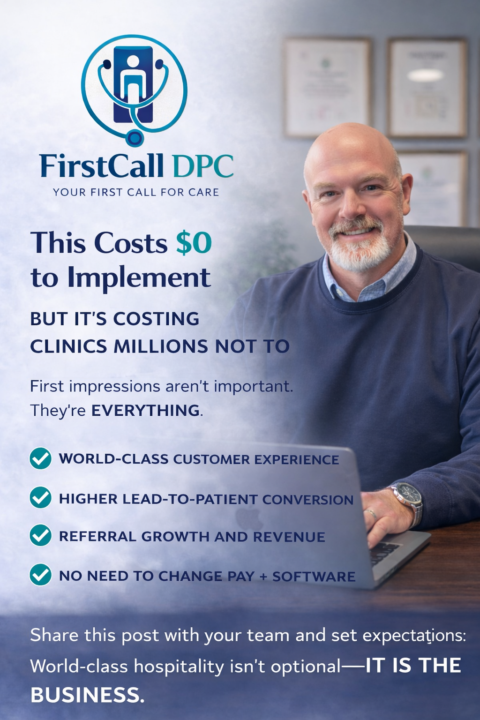
This Costs $0 to Implement — and It’s Costing Clinics Millions Not To This is not about an awkward script your staff has to memorize. It’s not about SEO hacks. It’s not about some magical unicorn platform promising “innovation.” In the next 7 minutes, you can implement something today: - with the team you already have - with your current pay structure - with your existing software - without buying anything But first, a true story. The $1,800 Phone Call That Exposed Everything A woman named Victoria on our team needed blood work. So did her partner. She asked where to go. I referred her to two clinics—both existing clients. - Clinic #1: ~$250 for consult + labs - Clinic #2: ~$900 for essentially the same thing Naturally, she called the cheaper clinic first. Call #1: put on hold Call #2: put on hold Call #3: “Hey, you’ve put me on hold twice and hung up twice.” Obligatory apology. Placed on hold again. She hung up. You would too. Then she called the $900 clinic. Her call was answered on the second ring. Warm greeting. Focused attention. Genuine interest in helping. They talked for 15–20 minutes. She scheduled labs for both people on that call. 💳 $1,800 paid over the phone, across the country, to a stranger. Not because of price. Because of experience. What the $250 Clinic Actually Lost (Without Knowing) They didn’t just lose $500 in initial revenue. They lost: - two long-term patients - future memberships - referrals - goodwill - and possibly their reputation In today’s world, bad experiences ripple outward. Any friend who asks Victoria for a recommendation will be told: 👉 “Go to the $900 clinic.” 👉 “Avoid the cheaper one.” This couple is affluent and influential. That goodwill damage compounds quietly—and brutally. And if she wanted to? She could’ve left a negative review saying: “They don’t answer the phone. They’re rude.” She’d be telling the truth. “They Were Just Shopping Around” — Exactly Yes. They were shopping around.
Zocdoc Isn’t the Problem. Misusing It Is.
This may be one of the most important conversations we have in this community. Zocdoc gets blamed a lot in DPC circles: - “Low-quality patients” - “Price shoppers” - “High no-show rates” - “Terrible ROI” Some of that criticism is fair. Some of it misses the point entirely. Let’s start with an honest question: What kind of patients actually use Zocdoc? In our experience, they tend to fall into a few buckets: - People who are frustrated with access - People who are new to the area - People who are used to transactional healthcare - People who believe “covered = cared for” (until it isn’t) - And yes—some are price shoppers That doesn’t make them bad patients. It makes them uneducated patients—and that distinction matters. Where practices get Zocdoc wrong Zocdoc is not: ❌ A relationship platform ❌ A loyalty channel ❌ A long-term acquisition engine Zocdoc is: ✅ A discovery tool ✅ A moment of intent ✅ A chance to redirect the patient journey The mistake happens when practices treat a Zocdoc booking like a win—when it’s actually just step one. How we re-framed Zocdoc inside FirstCall DPC We never built Zocdoc into our system as “marketing.” We built it as a controlled intake valve feeding into GoHighLevel. Here’s what that looks like operationally: 1️⃣ Zocdoc → GHL (email-based trigger) Since Zocdoc doesn’t fire webhooks: - Appointment emails route into GHL - GHL creates the contact - The workflow begins immediately 2️⃣ Immediate expectation setting Automatic SMS + email: - Confirms the appointment - Clearly states: This is Direct Primary Care We do not bill insurance Membership is required - Encourages early cancellation if it’s not a fit This alone filters a huge percentage of misaligned patients. 3️⃣ Speed + human touch - Staff attempts live contact quickly - Education > selling - If no response: 3 attempts Then cancellation No chasing. No begging. 4️⃣ Payment before care - Membership payment links sent via GHL - No payment = no visit - Automation handles reminders and cancellations
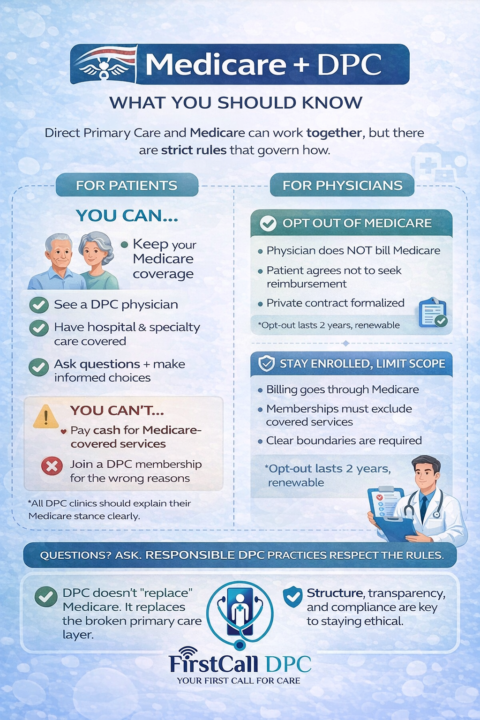
Medicare, Direct Primary Care, and the Rules No One Explains Clearly
One of the most misunderstood topics in Direct Primary Care is how DPC physicians interact with Medicare. Not because it’s shady. Not because it’s forbidden. But because the rules were written for a healthcare system that no longer exists. So let’s talk about it clearly. First: The Big Picture Medicare was designed around insurance billing. Direct Primary Care is designed around direct relationships. Those two models don’t naturally fit together—which is why Medicare has specific rules about how physicians can participate, opt out, or limit what they provide. Understanding those rules is critical—for doctors and patients. The Core Medicare Rule That Matters A physician who is enrolled in Medicare cannot charge Medicare beneficiaries cash for services that are otherwise covered by Medicare. That’s the foundation of the entire framework. From that single rule, everything else flows. The Two Legitimate Paths for a DPC Physician 1. Opt Out of Medicare A physician formally opts out and enters into private contracts with Medicare beneficiaries. - The physician does not bill Medicare - The patient agrees not to seek Medicare reimbursement - The relationship is entirely private - The opt-out lasts 2 years at a time This path is legal, structured, and commonly misunderstood. 2. Remain Enrolled, But Limit Scope A physician stays enrolled in Medicare but does not charge Medicare patients for covered services. - Medicare-covered services must be billed to Medicare - Non-covered services may be offered privately - Membership fees must be carefully structured - Boundaries must be extremely clear This path requires discipline and precise compliance. Why the Rules Feel So Rigid Medicare is designed to: - Prevent double billing - Protect beneficiaries from coercion - Maintain standardized coverage What it is not designed to do is accommodate innovative care models. So the rules aren’t malicious—they’re just outdated. Common Scenario Questions (And How DPC Doctors Stay Compliant)
0
0
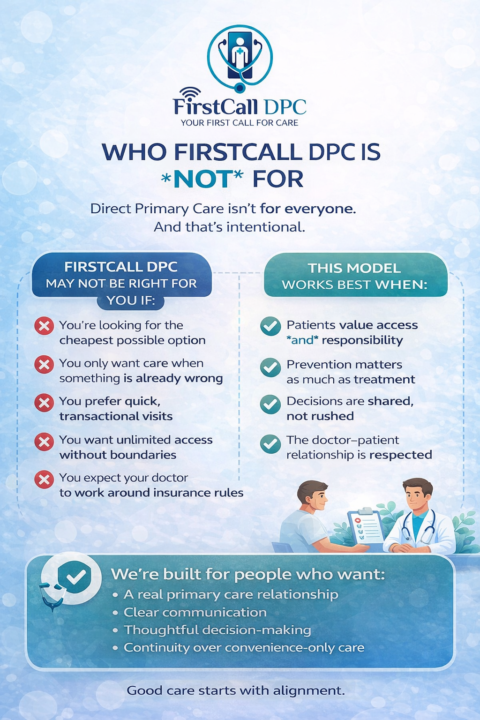
Who FirstCall DPC Is Not For
Direct Primary Care isn’t for everyone. And that’s intentional. FirstCall DPC may not be the right fit if: - You’re looking for the cheapest possible option - You only want care when something is already wrong - You prefer quick, transactional visits - You want unlimited access without boundaries - You expect your doctor to work around insurance rules This model works best when: - Patients value access and responsibility - Prevention matters as much as treatment - Decisions are shared, not rushed - The doctor–patient relationship is respected We don’t try to be everything to everyone. We’re built for people who want: - A real primary care relationship - Clear communication - Thoughtful decision-making - Continuity over convenience-only care If that resonates, FirstCall DPC tends to feel like a relief. If it doesn’t, that’s okay too. Good care starts with alignment.
1
0
1-4 of 4

skool.com/firstcalldpc
Direct primary care gives unlimited access to your doctor, same-day visits, clear pricing, and no insurance—medicine built on trust.
Powered by
