
Write something
🎉 MRCS Part B Success! 🎉
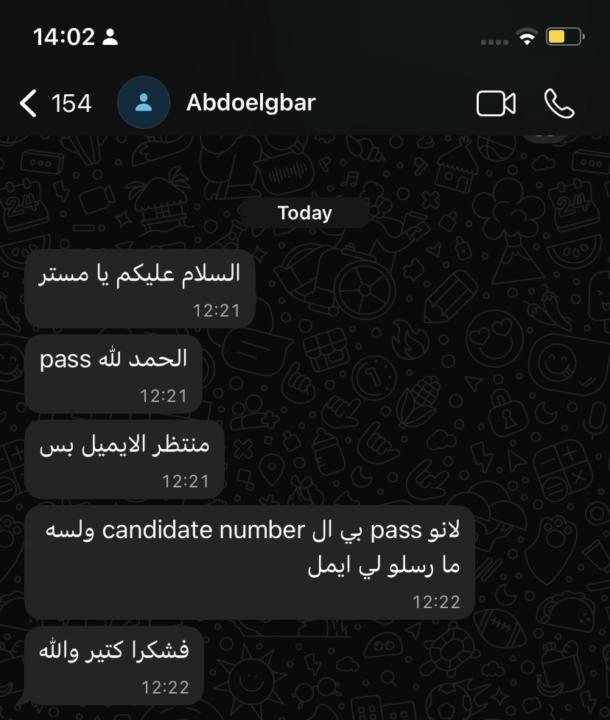
I am pleased to congratulate Alaa Aljamri, Abdoalgbar, and Abubaker on passing the MRCS Part B examination today. Many congratulations to you all, and I wish you continued success in your careers and in life. To all our other candidates, I wish you every success in passing this examination.
Congratulations
Congratulation Romeo for passing your exam @Romeo Chidziya
Congratulations to those who passed
We are thrilled to congratulate @Fathalrahman Gadallah @Mohammed Sadig for passing their Exam. Good luck with the rest of your journey.✅
New station added to pathology-Dermatology
🍄ACTINOMYCOSIS 🩺 Clinical Vignette A 25-year-old female with Crohn’s disease on steroids presents with a 4 cm ulcer on the face.On incision, you find greenish pus containing yellowish granules. ❓Q1. What is the most likely diagnosis? Actinomycosis — a chronic granulomatous infection caused by Actinomyces israelii, a gram-positive, anaerobic, filamentous bacterium. ❓Q2. What are the typical features of Actinomycosis? - Chronic, indolent infection with abscesses, fibrosis, and sinus tracts - Discharges thick pus with yellow “sulphur granules” - Mimics malignancy due to firm mass and tissue invasion ❓Q3. Where does this organism normally live? It is a commensal in: - Oral cavity - Gastrointestinal tract - Female genital tract ❓Q4. What are the risk factors? - Mucosal trauma (e.g. dental extraction, oral sepsis) - Steroid use / immunosuppression - Poor oral hygiene - IUD use (pelvic actinomycosis) - GI pathology – appendicitis, diverticulitis - Aspiration of oral secretions ❓Q5. What is the pathogenesis? 1. Mucosal barrier disrupted 2. Actinomyces invades deep tissues 3. Forms chronic abscess → fibrosis → sinus tracts 4. Sulphur granules represent bacterial colonies ❓Q6. What are the common sites of infection? SiteFeaturesCervicofacial (“Lumpy jaw”)Post-dental infection; firm jaw swelling with discharging sinusesThoracicAspiration from oral cavity → chronic pneumonia or abscessAbdominal / PelvicFollows bowel perforation or IUD; may mimic malignancyCNSSecondary spread causing brain abscessMandibleOsteomyelitis after trauma/dental surgery ❓Q7. Why can Actinomycosis mimic malignancy? Because it causes a firm, fibrotic, slowly enlarging mass that invades adjacent tissues and forms fistulae. ❓Q8. What are the characteristic findings at surgery? - Greenish pus with yellow “sulphur granules” - Dense fibrotic tissue and sinus tracts - Granules seen in < 50 % of cases - Culture confirmation needed (slow-growing anaerobe) ❓Q9. How is the diagnosis confirmed?
8
0

1-30 of 42
powered by

Suggested communities
Powered by

